 The coronavirus pandemic has tested our healthcare system like never before, and physicians are leaning on imaging providers to provide diagnostic testing for patients who are expected to have or are suffering from the virus.
The coronavirus pandemic has tested our healthcare system like never before, and physicians are leaning on imaging providers to provide diagnostic testing for patients who are expected to have or are suffering from the virus.
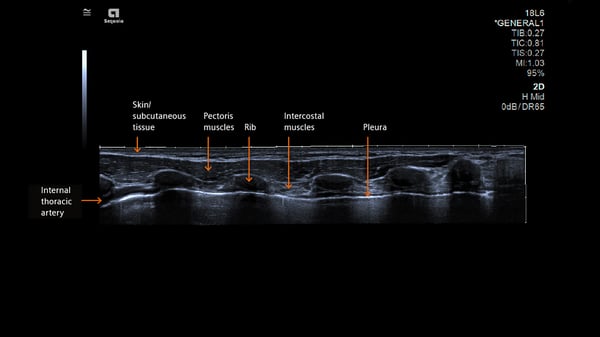
One area that’s started to gain more attention in diagnostic protocols is ultrasound. That’s because lung ultrasound can:
- Determine Normal Lung by demonstrating A Profile of a dry lung
- Determine Pneumothorax by demonstrating the air between layers prevents sliding.
- There are references that state ultrasound has a 99% predictive value for pneumothorax
- Determine Pulmonary Edema by demonstrating B lines of wet lungs
- Determine Pneumonia/consolidation routinely in pediatrics with some limitations in adults
- Determine pleural effusion easily
There are four key reasons why ultrasound is being used in this regard.
- Bedside Testing
Thanks to the compact and highly mobile nature of most ultrasound systems, it’s possible to conduct the exam without needing to move the patient. Instead, you can bring the screening to them. This reduces patient complications stemming from transport and limits the risk of infection to others that would otherwise increase when the patient is moved to a separate testing site.
- Non-Invasive
One of the main benefits of all ultrasound testing is in its non-invasive nature. This is particularly true for COVID-19 cases, where keeping patients comfortable and stable is critical.
- No Radiation
CT and X-ray, the two modalities most commonly used for lung diagnostics related to COVID-19, each expose the patient to radiation at a time when they may already be in serious or critical condition. The effect of these standard amounts of radiation certainly isn’t thought to be harmful, but there also haven’t been widespread studies related to their effects on patients suffering from significant progression of the virus. And because a COVID patient may need to submit to multiple screenings over the course of their inpatient stay, any opportunity to avoid additional radiation exposure is typically one worth taking advantage of.
- Disinfection
Generally speaking, an ultrasound system and transducer will be far easier to disinfect than an entire CT system, the room it’s in and the wheelchair or gurney used to transport the patient to their exam. This saves time, resources and, yet again, reduces potential exposure to staff and other patients.
Let’s look more closely at how lung ultrasound is making its mark.
 Lung Imaging White Paper
Lung Imaging White Paper
By using thoracic ultrasound on patients, the physician can closely monitor the the lungs and pleural space. This allows them to more effectively triage patients as necessary, determining which cases require immediate intervention and which might benefit from further monitoring.
Siemens Healthineers has released a fantastic White Paper outlining the mechanics of testing and the specific reasons why lung ultrasound has become so important. I highly recommend you check it out. Not only does it provide background on the clinical uses of ultrasound, but it also delves into the history of lung sonography, the types of artifacts to watch out for, and how to properly set up the transducer and progress through your sequences.
Equipment Choice
Because it’s considered a point-of-care exam that can take place right at the bedside, just about any ultrasound system could be used for a lung exam. Smaller, more portable systems, however, are a lot more common.
In the Siemens Healthineers product line, that means you’d be far more likely to utilize the ACUSON Bonsai or ACUSON P500 cardiovascular system due to its suitability for routine diagnostic procedures and its high rate of portability. A system like the ACUSON Redwood, which offers advanced clinical capabilities and adaptability across numerous departments, could certainly be used, but it isn’t strictly necessary in order to accomplish the type of lung examination needed to assess COVID-19 progression.
Transducer Choice
A curved transducer is going to be the most common transducer for this type of screening.
Infection Control
 One of the key benefits of ultrasound is the relative ease of infection control in comparison with other diagnostic tools. But proper infection control does still require certain procedures to be followed.
One of the key benefits of ultrasound is the relative ease of infection control in comparison with other diagnostic tools. But proper infection control does still require certain procedures to be followed.
First, you’ll want a list of approved disinfectants, ones that are simultaneously capable of reducing viral exposure and protecting your equipment from hardware failure. If you have a Siemens product, you can use this list of approved disinfectants for transducers to get started.
In addition, here is a handy guide that offers specifics about the ways to keep your transducer safe and sterile in between patient exams. Among the key takeaways:
- Do not immerse the transducer in any disinfectant for longer than an hour
- Don’t rely on hot steam, cold gas or Ethylene Oxide
- Don’t be abrasive: Abrasive cleaning agents and organic solvents can actually do damage to the transducer and lead to compromised image quality.
Finally, don’t forget to apply proper disinfectant procedures to the system itself. You’ll want to once again use an approved disinfectant, making sure to target all surfaces, with particular attention placed on the trackball, soft keys, knobs, and really anywhere you make regular contact with. Ensure you’re taking care to prevent fluid from actually leaking into the system itself through small openings such as those on the control panel or the keyboard.
Head here for more ultrasound disinfectant insights and, for further guidance on infection control in the COVID-19 era, feel free to consult your imaging system infection control guide.
Separation of Patient States
Another benefit of ultrasound imaging that you ought to remember: by using ultrasound, with its mobility, accuracy and relatively simple disinfection procedures, it’s easier to separate your patient populations into COVID cases and everyone else.
Not all facilities have the resources to dedicate an entire X-ray room or area of the hospital to COVID patients, which might mean the custodial team needs to go in after each patient and initiate a thorough deep clean of the area before the next patient can come in. This is a time-consuming process, but many organizations simply don’t have a choice.
If some things can be accomplished with ultrasound, you can free up other resources, such as your CT systems, to be used for the highest-risk patients or, if you can swing multiple X-ray rooms, for patients not presenting with COVID symptoms. Leaning on ultrasound during this time is a straightforward way to maximize resources at your facility while reducing exposure of patients and staff members to infection.
The Situation Continues to Evolve
It’s a brave new world we’re living through right now, and no doubt clinicians will continue to come up with innovative ways to provide optimal care and reduce infection risk. Ultrasound, which we weren’t hearing a lot about at the start of the pandemic, may turn out to be one of those innovations if what we’re hearing from our colleagues in Italy and Germany is any indication.
Please reach out to me if you have any questions about disinfection, lung ultrasound, or anything else. I’d be happy to help. And if you have your own insights you’d like to share with the imaging community, please comment on this article!










Comments